Throughout the state of Ohio in medical practices and hospitals, Medicaid or Managed Medicaid plans are the lowest dollar payers. The reimbursement rates typically do not cover the cost to provide care. For years, Commercial Insurance rates have been negotiated to rates higher than Medicare, typically between 106-125% of the current year Medicare Physician FFS. These rates have helped medical practices and hospitals continue their care for the indigent population.
By stark contrast, behavioral health practices can receive rates through Ohio Mental Health and Addiction Services (OMHAS) at significantly higher rates than Commercial payers – rates that are almost 100% of the Medicare fee schedule. This makes Medicaid and Medicare the best payers. Medicaid and the Managed Medicaid plans are not only the highest dollar payer, but they pay for many services, such as RN and LPN medical services. that the Commercial plans will not cover and offer superior speed and efficiency when processing claims.
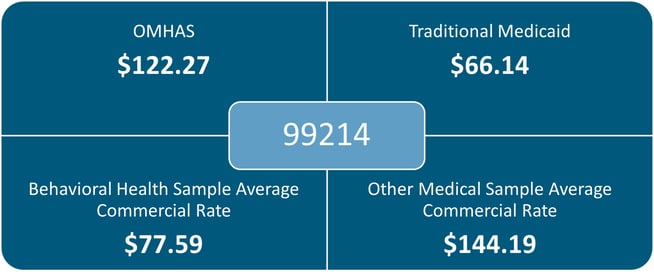
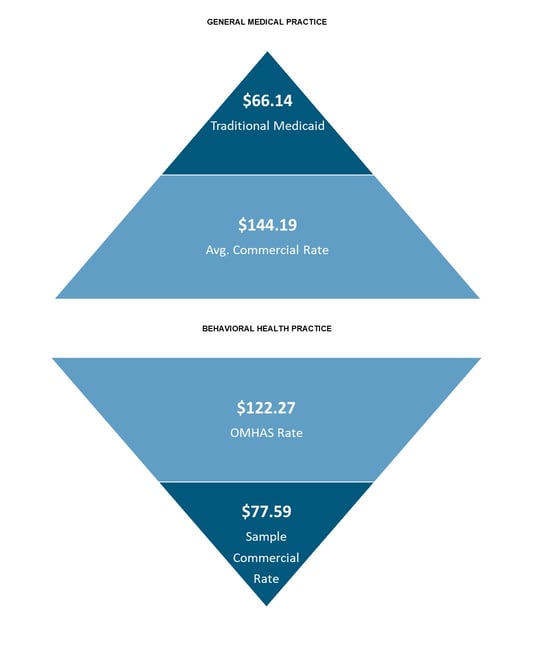
Using an established evaluation and management code for a level 4 visit shows the contrast between the rates that behavioral health and general medical practitioners face. The difference between what an OHMAS provider and a general medical practice receive from Traditional Medicaid is approximately $56 or 85%. In contrast, a sample commercial rate for a general medical practice and a behavioral health provider is about $67 less or about 47%.
Example 1:
Example 2:
 The above disparity in reimbursement rates has created a situation with limited access for commercially insured patients for behavioral health services. Many payer mixes at behavioral health provider organizations are 90% or higher Medicaid patient volume, leaving very little access for commercial, self-pay or other pay patients.
The above disparity in reimbursement rates has created a situation with limited access for commercially insured patients for behavioral health services. Many payer mixes at behavioral health provider organizations are 90% or higher Medicaid patient volume, leaving very little access for commercial, self-pay or other pay patients.
Below is a topline look at the numbers within the state of Ohio:
- 11,680,000 Ohioans (2020)
- 2,336,000 (1 in 5) Ohioans need or will have a need to access behavioral healthcare
- 3,000,000 Ohioans are covered by Medicaid
- 8,680,000 Ohioans are covered by another payer type
- 500,000 Ohioans are covered by Medicaid receiving behavioral health services
Factoring the number of Ohioans that are covered by a payer source outside of Ohio Medicaid, there are an estimated 1,736,000 patients that need or will need behavioral health and addiction services.
As our communities continue to see an increase in need for behavioral health and addiction service treatment options, it will be paramount to address the inequities in access to care. With the mental health events in the news and addiction-related deaths at every turn, we as providers must come together with new solutions in pursuit of the Triple Aim: High Quality Care, High Value Patient Experience and Lower Cost.
A study published in the Journal of the American Medical Association shows that patients treated in advanced Value-Based care models are 5.6% less likely to experience hospitalizations and 13.4% less likely to need emergency room visits. Recent cost data shows that a behavioral health or addiction related emergency department visit costs on average $573 per visit. There is an average cost of more than $8,000 for a behavioral health inpatient episode, with higher acuity stays costing more than $8,900 and including eleven days of inpatient care (Consumer Health Ratings).
The imbalance in access for patients who require medical help for their behavioral health and addiction needs has created the perfect environment for behavioral health organizations and providers across the state to come together in the interest of high-quality, highly accessible care. Providers can come together and explore opportunities to demonstrate their value to the commercial insurance payers and work towards Value-Based care and reimbursement strategies with a wider variety of covered services. The value strategies that have been used in the primary care and family medicine markets are the same in behavioral health. If the patient can be managed within an outpatient office setting, or in some cases within the patient’s home, they are less likely to have acute exacerbations of their illnesses or diseases that lead to costly emergency room visits and inpatient admissions.
Along these same lines, there are opportunities being discussed across the state that would create tighter, more streamlined care relationships between primary care and behavioral health providers. These types of arrangements may have many different faces with the ultimate goal of providing high-quality, low-cost care for patients.
A Value-Based model is needed in today’s healthcare space and presents a unique opportunity to achieve both mission and business goals. The successful behavioral health organizations of the future will need to navigate both exceptional patient care and a model of Value-Based care. Our prediction is that integrated behavioral health ACOs will be at the center of this clinical and financial success.